IVF Treatment Cost in Srinagar
If you are finally planning to undergo IVF treatment in Srinagar, you must be bombarded with many questions, such as what the IVF treatment cost in Srinagar is. Is affordable IVF package treatment available in Srinagar? What is the cost per IVF cycle? Is the success rate high?
Then we at Imprimis IVF, the best IVF treatment centre in Srinagar, are here to help you search for the cost of IVF in Kashmir.
Cost of IVF in Srinagar
Depending upon the couple’s medical conditions, challenges, expertise, and experience, IVF costs in Srinagar are between 1,00,000 and 2,75,000 INR. However, there are no fixed IVF charges in Srinagar, Jammu, and Kashmir regions. IVF costs in Srinagar vary from clinic to clinic.
Factors Affecting IVF Costs
A bunch of factors affect IVF cost in Srinagar in a particular area. Let’s walk you through them one by one.
Type of IVF Treatment-:
With medical advancements, IVF is further classified into various types to summon the best results and increase the success rate.
We provide the following types of IVF Treatment in Srinagar:
Natural IVF
As the name suggests, Natural IVF doesn’t involve any stimulation drugs. Owing to this, the cost of medications is significantly low in the case of Natural IVF.
On average, the Natural IVF treatment in Srinagar can cost about 50,000 INR.
IVF + Egg Donor
In this IVF treatment, the embryos of a fertile woman are collected and transferred to the fallopian tube of the female who has a problem conceiving.
The cost of finding an egg donor may range between 35,000 to 60,000 INR. The entire donor egg IVF cost is around 1,50,000.
IVF + Frozen Embryo Transfer (FET)
This IVF cycle involves thawing one or more frozen embryos and implanting them in the uterus.
The average cost of IVF+FET is around 50,000 to 70,000 INR.
IVF + Donor Sperm
During this IVF process, the sperm of a donor are collected and placed into the female’s uterus around the time of natural ovulation. Finding a sperm donor may cost a couple around 10,000 to 20,000 INR.
IVF + Intracytoplasmic Sperm Injection (ICSI)
This IVF treatment involves the injection of a single sperm into the cytoplasm of a mature egg, which results in pregnancy.
The average ICSI treatment cost may lie between 70,000 and 3,00,000 INR.
Mini IVF (Minimal Stimulation)
Mini IVF or minimal stimulation involves mild drug stimulation during the first stage of IVF. The average cost ranges between 70,000 to 80,000 INR.
Depending on which IVF treatment suits you the best, IVF charges may vary. Your location also plays a crucial role in deciding IVF treatment prices, as the cost per IVF cycle may vary from city to city in a particular state.
The Number Of IVF Cycles-:
Due to various reasons, couples do not succeed in conceiving in just one IVF cycle. The cost per IVF cycle is about 1,50,000 INR. The higher the number of IVF cycles, the higher the IVF treatment cost in Kashmir.
Cost of IVF Injections-:
IVF medications are mainly provided in pills and injections during the first stage. During the entire IVF treatment, various medicines are to be taken by the couple as per the prescription of the IVF experts. The IVF injections cost between 60,000 and 80,000 rs.
Armed with medical expertise and top-notch medical infrastructure, we at Imprimis IVF, the Best IVF Centre in Srinagar, offer the best medical assistance to help you embark on your journey of parenthood.
What are the reasons behind Infertility?
Problems in conceiving a baby may result from male or female Infertility and, in some cases, due to both.
Female Infertility takes into account various medical issues:
- Blocked Fallopian Tubes
- Thyroid Problems
- Ovulation Disorders
- Endometriosis
- Irregular Periods
- PCOS
- Premature Menopause
Male Infertility may be caused by the following:
- Sperm Cramps
- Azoospermia
- Oligospermia (low or poor-quality sperm)
- Hormonal Imbalances
- Testicular Inflammation
- Varicocele
- Klinefelter Syndrome (a genetic condition)
- Ureaplasma
- Gonorrhea
Depending on the root cause, different reproductive technologies are assigned to help achieve pregnancy. These medical technologies are referred to as Assisted Reproductive Technologies.
Assisted Reproductive Technologies are classified into various types, which include:
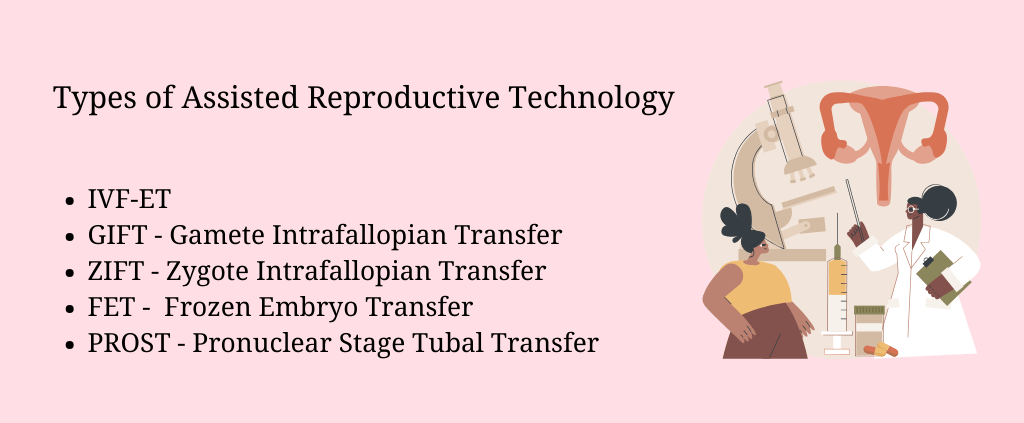
- IVF-ET
- GIFT – Gamete Intrafallopian Transfer
- ZIFT – Zygote Intrafallopian Transfer
- FET – Frozen Embryo Transfer
- PROST – Pronuclear Stage Tubal Transfer
IVF is the most commonly employed Assisted Reproductive Technology (ART) because of its high success rates. IVF has successfully tackled the problems faced in conceiving a baby in women with blocked fallopian tubes and men with low or poor-quality sperm.
Let’s dive into the five stages of IVF and how affordable IVF treatment is rekindling the flame of conceiving a baby amongst couples with no success, even after endless efforts.
Success Rates of IVF Treatment
With medical advances, the success rates of IVF have seen a rising trajectory. It has proven to be a boon for women over 40 trying to conceive. The live birth rate for the IVF cycle has also witnessed a sharp increase.
Your dream of welcoming a tiny human being is possible! We wholeheartedly welcome you at Imprimis IVF, Srinagar!