Freezing of Eggs, Embryos, and Sperms: All You Need to Know About Cryopreservation!
The ability to freeze embryos has emerged as a powerful tool. This process, known as cryopreservation, offers individuals and couples a chance to defy the traditional biological clock, allowing them to preserve their fertility for a future pregnancy. The chance to delay parenthood is a relatively new phenomenon.
Medical advances such as cryopreservation, freezing and storing gametes and embryos for later use, allow individuals and couples to control their family planning schedules. This article introduces the world of cryopreservation and explores its applications, benefits, and considerations.
Why is Cryopreservation an Emerging Trend?
Cryopreservation is no longer a futuristic concept but an established medical practice. Infertility centres in and around the world are interested in freezing eggs, sperm, and embryos.
Social factors such as higher education, career aspirations, or simply a desire to find the right partner lead people to preserve their fertility for a future pregnancy. The decision to freeze eggs, sperm, or embryos is quite, personal.
As a process, cryopreservation is an expensive process & medical insurance may not cover fertility treatments, so you must consider your goals & discuss them thoroughly with your partner, before making this decision.
Why Should You Opt for Cryopreservation?
You must be wondering, why cryopreservation has been an emerging trend suddenly & why is everyone talking about it. Let’s dive into some reasons:
1. Body Clock
As we age, our fertility naturally declines. Think of eggs and sperm as superheroes because they’re the strongest when they’re young. Cryopreservation allows you to freeze eggs and sperm at their peak, giving you a better chance of getting pregnant later.
2. Medical struggles:
Cancer treatment can be hard on the body, including our reproductive system. Cryopreservation offers hope because it allows you to freeze whole eggs or sperm before treatment so you can have a family after recovery.
3. Finding Your True Self
Gender reassignment can affect fertility. Cryopreservation allows transgender people to preserve their ability to have children before hormone therapy or surgery.
4. Waiting for the right time
Maybe you’re busy building your career or haven’t found the perfect partner yet. Cryopreservation gives singles and couples the flexibility to freeze eggs, sperm, or even embryos so they can start a family when they are ready.
Does Freezing Damage Embryos?
A persistent question often arises: Does freezing harm embryos? The answer is that, like many things in science, it is not a simple yes or no.
Cryopreservation is a time- and temperature-sensitive process, and while the technology has continued to advance, there are inherent risks. Freezing can damage embryos, and thawing them later can also damage them. If multiple embryos are frozen, some or all may not survive the process, so choosing the right infertility centre is essential!
What is the Process of Cryopreservation?
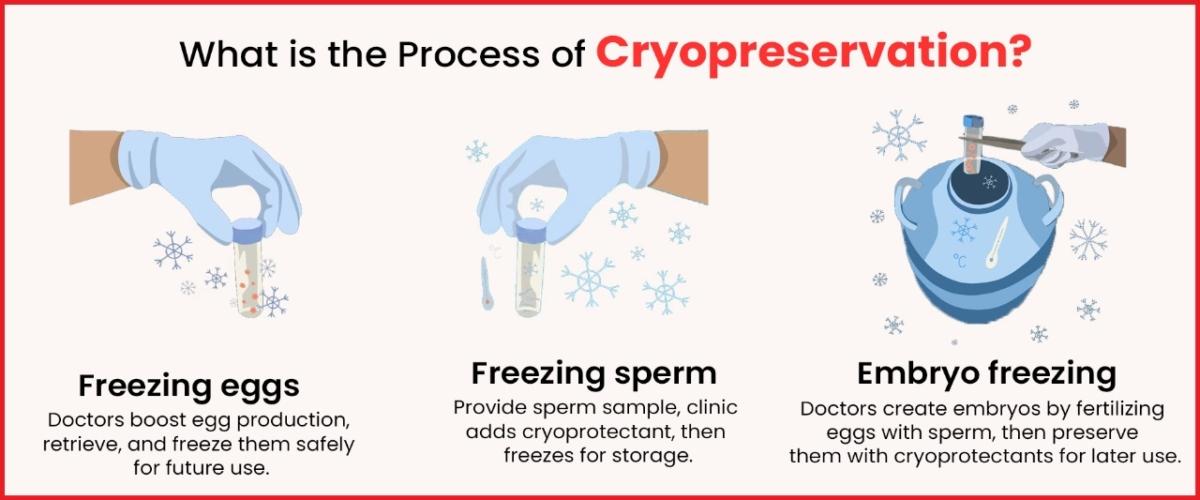
Imagine taking a break from planning your baby! This is what cold storage does. Here’s a simplified version:
1. Freezing Eggs
Think of it like putting eggs on ice. Doctors will give you medicine to make your ovaries produce more eggs. They then remove the eggs quickly and easily. Before storing them in a very cold freezer with a special antifreeze, they make sure they won’t be damaged by freezing.
2. Freezing sperm
It’s pretty simple. You provide a sperm sample and the clinic adds a special “antifreeze” to protect it. It then goes into the same ultra-cold freezer as the eggs.
3. Embryo freezing
It’s like putting in a little miracle. Doctors fertilize eggs with sperm in the laboratory and create embryos. These early embryos receive the same antifreeze treatment and super cryopreservation as eggs and sperm.
How Long Can Embryos Be Stored?
Imagine putting your family planning on hold for ten years! You can do this by freezing embryos. Most clinics recommend keeping them in the freezer during this time to give you flexibility. But here’s the great part: ten years is not a deadline. If you need more time, you can extend the storage.
If you want to preserve your eggs, sperm, or embryos, get in touch with Imprimis IVF Srinagar, our experienced doctors will guide you through the process in detail.
What can be Done in the Case of Separation from the Partner?
Embryos are created from sperm and egg. Therefore, sperm and egg providers must agree separately on the conditions of storage of embryos. Both the female as well as male partners (unless donor eggs or sperm are used) must complete a special consent form expressing their wishes regarding the use of the stored material.
Embryos can only be used if both male and female partners agree to the intended use. It’s also important to agree on what you want to do with the embryos if one of you faces mortality.
Going through these problems might be quite overwhelming, but don’t worry. The experienced team of professionals, counsellors, doctors, and staff at our infertility center will make you feel at ease. You can visit here to study the proper guidelines for the procedure.
Understanding the Risks & Benefits of Cryopreservation
Cryopreservation is like all medical procedures, It has its own considerations. Although freezing and thawing techniques have become increasingly successful, there is always the possibility that cells or embryos won’t survive the process. Also, cold storage and high costs could also be a major factor. However, the benefits often outweigh the risks.
Cryopreservation offers an opportunity to preserve fertility and give individuals and couples more control over their family planning decisions and choosing the right infertility centre is crucial. Pregnancy success rates with frozen eggs, sperm, and embryos continue to improve which makes it a viable option for many people.
Frequently Asked Questions
1. Is cryopreservation right for me?
A consultation with a fertility specialist at the Fertility Center is essential. You can also contact us at 7678556881 and we can assess your individual situation and discuss whether cryopreservation is compatible with your family planning goals or not.
2. What is the success rate of Cryopreservation?
Success rates depend on factors such as the age of freezing and the reason for cold storage. Your fertility specialist at Imprimis IVF can provide you with personalized statistics based on your circumstances.
3. What happens to unused frozen eggs, sperm, or embryos?
You always have the option to donate them to research or help another couple struggling with infertility.
Takeaway
Cryopreservation is a powerful technique that empowers individuals and couples to make informed choices about their reproductive future. By understanding the process, and its pros and cons, you can make decisions that align with your personal vision of parenting. We at, Imprimis IVF Srinagar, are dedicated to delivering exceptional results at our infertility centre and keeping the candle of hope burning for many people.