IVF Diet Chart – Foods to Eat During IVF Treatment
IVF Diet Chart – In-vitro fertilization treatment offers a 30-40% success rate for women of fertile age. IVF experts have concluded that diet has no significant contribution to deciding the success rate of IVF treatment. However, it affects the quality of the eggs the ovaries produce and the overall reproductive health. It would help if you stuck to a diet chart and a healthy lifestyle to succeed in your IVF treatment.
Gut health and healthy defection are decisive elements of conception and healthy pregnancy. To ensure the proper upkeep of reproductive health, consuming a diet rich in micronutrients and macronutrients is vital.
The first step is to increase the number of meals you take and break every meal into smaller ones. So it’s advised to take five meals in a day! Yes, you heard it right. Make sure that you cover all the essential nutrients.
Some Strict IVF Diet Chart during IVF Treatment.
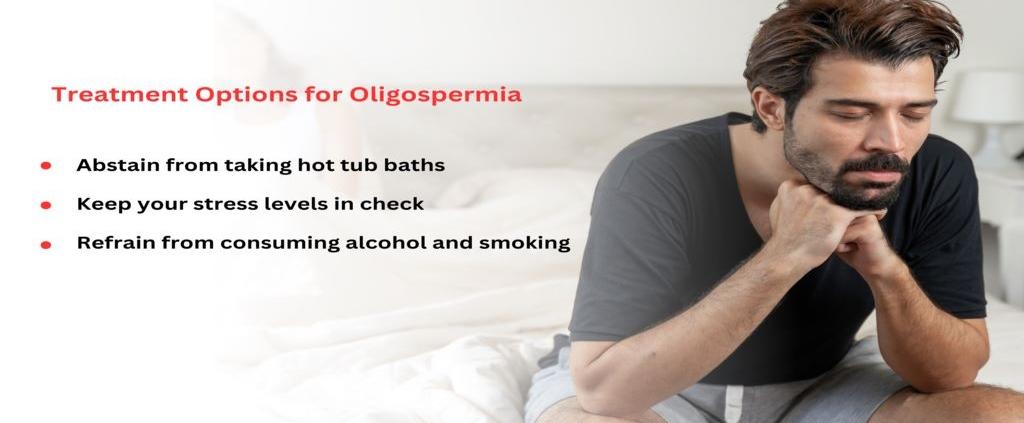
Before moving ahead to the diet chart to follow during IVF, it is advised that you steer clear of smoking and drinking. Medical evidence has cemented that consumption of alcohol and smoking hampers the process of egg maturation, which results in chromosomal abnormalities. Also, regular and excessive consumption of alcohol and tobacco further causes problems in conceiving and carrying the pregnancy to term.
Apart from smoking and drinking, reproductive specialists also advise limiting caffeine intake to one to two cups or 200 mg daily to stay safer. Also, the female partner should not consume energy drinks containing caffeine during IVF.
Foods to Eat during IVF Treatment
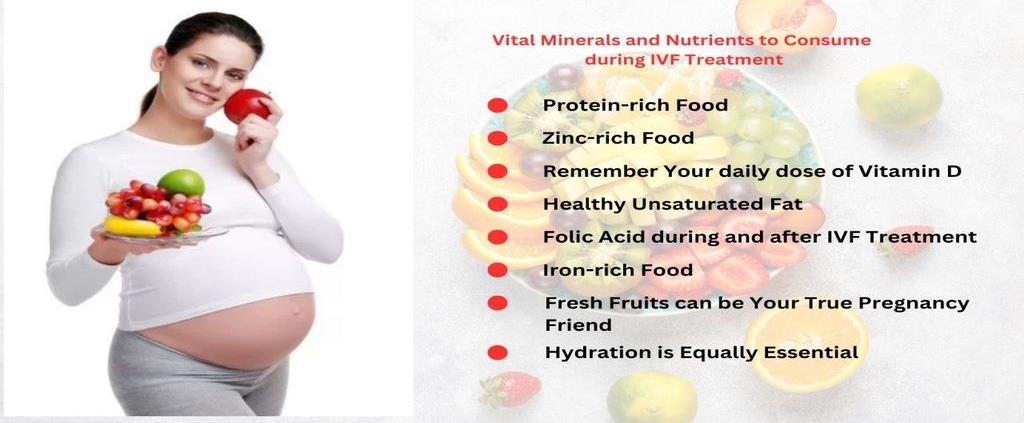
1. Protein-Rich Food-:
Apart from being the body’s building blocks, proteins also help in the ovulation process and the development of eggs in the female. Dairy products, well-boiled eggs, yoghurt, soya, broccoli, lentils, and meat contain numerous proteins. Doctors recommend that a woman, during her IVF treatment, consume 60 grams of protein in her daily diet.
2. Zinc-Rich Food-:
Zinc plays an essential role in maintaining the balance of hormones and ovulation. A woman should consume around 15 milligrams of zinc-rich food during the day. Dairy products, whole grains, beans, breakfast cereals, sesame seeds, flax seeds, kidney beans, and nuts are excellent sources of zinc that the woman should consume during IVF treatment.
3. Remember Your daily dose of Vitamin D-:
Vitamin D helps produce good-quality eggs that can be used for IVF. So, a woman needs to consume vitamin D, which is present in cow’s milk, cod liver oil, fortified cereals, soy milk, etc.
4. Healthy Unsaturated Fat-:
Harvard School of Public Health finds that a diet containing healthy unsaturated fats like avocados and olive oil helps boost live birth rates.
5. Folic Acid during and after IVF Treatment-:
Folic acid plays a vital role in developing a child’s brain and spinal cord. To ensure their proper formation, 400 mcg of folic acid, found in green leafy vegetables, should be consumed by the female partner during IVF treatment.
6. Iron-Rich Food-:
Iron plays a significant role in maintaining the health of the eggs and ovulation. Reproductive specialists say that a woman, during her IVF treatment, should consume more than 27 grams of iron in the form of green leafy vegetables, pumpkin seeds, oysters, spinach, and beans daily. Make sure that your per-day iron intake should not exceed 45 grams.
Iron deficiency can cause anaemia, reduced libido, oxidative damage to ovulation, and may also lead to premature births or a pretty small baby.
7. Fresh Fruits Can Be Your True Pregnancy Friend-:
Fruits like bananas and pineapples are quite beneficial in a woman’s pregnancy journey. Bananas are a great source of vitamin B6, essential for the healthy regulation of periods. Pineapples are rich in manganese, which helps in the nutritious secretion of reproductive hormones.
8. Hydration is Equally Essential-:
Any IVF diet chart stands complete with adequate water intake. 6-8 glasses of water a day will help prepare the uterus for embryo implantation by thickening the uterine lining. It’s also crucial to keep your water intake in check to ensure proper digestion and circulation of the above-mentioned essential vitamins and minerals during IVF treatment.
Summing up the IVF Diet Chart
Imprimis IVF, the best IVF centre in Srinagar, has summed up all the food sources consisting of the nutrients mentioned above that will serve as a boon in your IVF journey-:
- Fruits like bananas, pomegranates, and pineapple
- Vegetables like cabbage, broccoli, and potatoes
- Fresh green leafy vegetables
- Other fresh citrus fruits and vegetables
- Avocados and corn
- Beetroot and sweet potato
- Low-fat dairy products and water
- Nuts (a rich source of omega-3 fatty acids and protein) and berries
- Whole grains, legumes (chickpea, soybean, pea), beans, and lentils
- Lean meat and salmon
Diet alone may not be able to fulfil all your dietary needs during IVF treatment, so the doctors may advise you to take some multivitamin supplements to prepare your body for the journey.
Foods to Avoid During Your IVF Treatment
Now that you have a good idea of the foods you should include in your diet during your IVF journey, it’s equally important to know the foods that must be kept at bay.
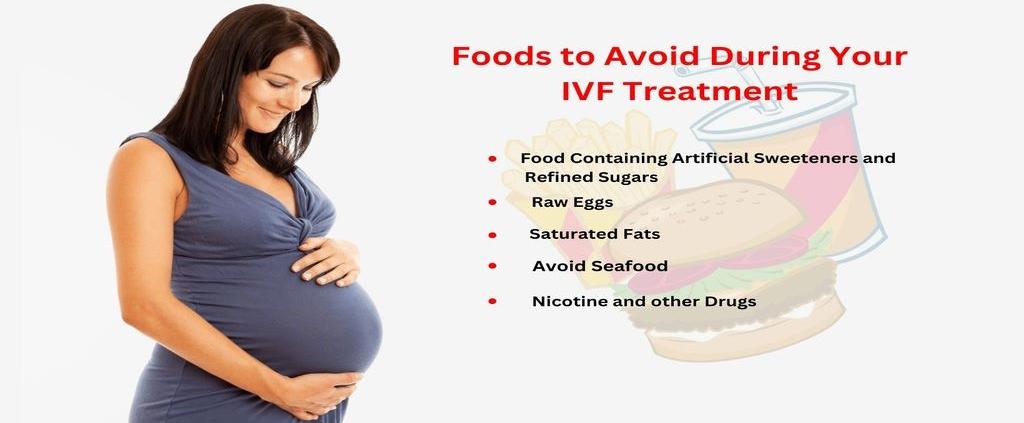
1. Food Containing Artificial Sweeteners and Refined Sugars-:
Artificial sweeteners and refined sugars negatively affect conception. So, it is advised to women undergoing IVF treatment to stick to healthy sugars and avoid bakery products like biscuits and cakes.
2. Raw Eggs-:
It is advised to avoid consuming raw eggs, which are present in processed food products like mayonnaise and salad dressing, as it may lead to food poisoning.
3. Saturated Fats-:
Doctors have found that food containing saturated fats can hamper conception by lowering the number of eggs used for fertilization in IVF. Foods containing high levels of saturated fats include white rice, cheese, butter, and fatty processed meats.
4. Avoid Seafood-:
Although seafood is packed with the goodness of essential fatty acids and proteins, it also contains mercury. Mercury present in tuna and mackerel can lead to complications in the growth of the fetus and may also lead to congenital disabilities.
5 Nicotine and other Drugs-:
As already mentioned, smoking and drinking are strictly prohibited during IVF. A woman should also stay away from nicotine and other drugs.
Avoid sodas, spicy junk food, pickles, vinegar, unpasteurized milk, and canned and processed food.
Is it true that IVF Treatment will be Successful in the first go?
It is a common misconception that couples have about IVF treatment. But the fact is that no fertility treatment centre can guarantee a 100% success rate. The medical expertise and infrastructure required for IVF treatment vary from clinic to clinic.
However, reproductive specialists worldwide have advised specific preventive measures that a couple can follow to welcome a healthy baby in a minimum number of IVF cycles.
The Right IVF Clinic will help Increase Your Success Rate-:
In-vitro fertilization is a highly complicated Assisted Reproductive Technology.
The right clinic will offer you a promise of excellent medical expertise and state-of-the-art lab fertility technology like Imprimis IVF, the best IVF centre in Srinagar can help increase your success rate by a good percentage. So, consider all the necessary things before finalizing your IVF fertility centre.
Keep Your Dosage and Medication Timing in check-:
Don’t skip your hormonal medications at any cost. Ensure that you take your IVF pills and injectibles at the right time.
Say No to Strict Bed Rest-:
After any medical treatment, the doctor advises you to rest and give your body time to heal. It would be best if you did the same after embryo transfer. However you must understand that IVF treatment differs entirely from other medical procedures.
The doctor will not advise strict bed rest for you. The reason behind this is that when your brain is inactive.
Positivity and Faith in the Process are Equally Important-:
A couple should never forget that positivity and complete confidence in the IVF treatment will serve as a pillar to bring positive pregnancy results.
Conclusion about IVF Diet Chart
Avoid making any drastic changes in your diet when it comes to food. It’s best to consult a reproductive specialist before IVF treatment to choose the best diet plan that suits your needs. If you are looking for the best yet affordable IVF treatment in Srinagar, we wholeheartedly welcome you at Imprimis IVF, Srinagar.