Unexplained Infertility: Tests, Diagnosis & Treatment
Infertility is often a silent struggle that affects millions of couples worldwide. For many, medical science can pinpoint the cause, hormonal imbalance, poor sperm quality, blocked fallopian tubes, or ovulation disorders. But for some couples, even after a thorough medical evaluation, no specific cause can be found. This condition is known as unexplained infertility, and it can be one of the most frustrating diagnoses in reproductive medicine.
In this article, we’ll break down everything you need to know about unexplained infertility, including the possible reasons, diagnostic tests, emotional impact, and treatment options that can help couples achieve pregnancy.
What Is Unexplained Infertility?
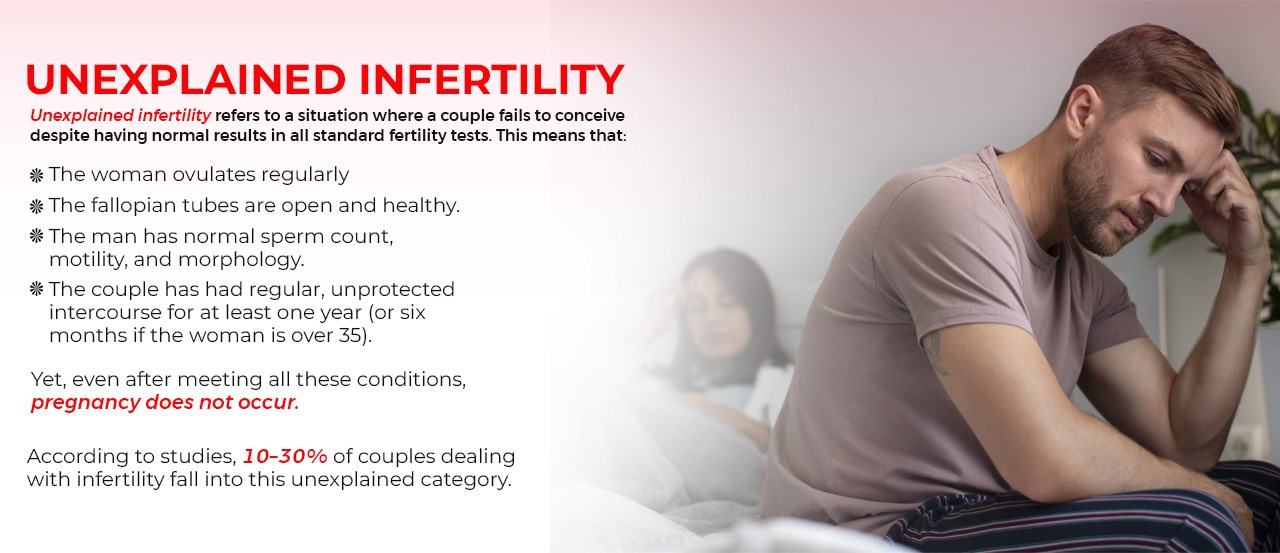
Unexplained infertility refers to a situation where a couple fails to conceive despite having normal results in all standard fertility tests. This means that:
- The woman ovulates regularly.
- The fallopian tubes are open and healthy.
- The man has a normal sperm count, motility, and morphology.
- The couple has had regular, unprotected intercourse for at least one year (or six months if the woman is over 35).
Yet, even after meeting all these conditions, pregnancy does not occur.
According to studies, 10–30% of couples dealing with infertility fall into this unexplained category.
Why Does Unexplained Infertility Happen?
While medical tests may appear normal, subtle biological factors could still affect conception. Some possible hidden causes include:
Egg Quality Issues:
Even if ovulation occurs, the egg may not be healthy or mature enough for fertilisation. Poor egg quality often becomes more common after age 35.
Sperm Function Problems:
Sometimes sperm count and motility look fine in a lab test, but the sperm might fail to fertilise the egg due to molecular or DNA-level abnormalities.
Fertilization Problems:
There could be a failure in the interaction between sperm and egg, preventing the sperm from penetrating the egg membrane.
Embryo Development Errors:
Fertilisation may occur, but the embryo fails to develop properly, preventing implantation in the uterus.
Uterine Receptivity Issues:
Even a healthy embryo can fail to implant if the uterine lining (endometrium) isn’t receptive or the timing of implantation is off.
Immune or Genetic Factors:
Sometimes the body’s immune system mistakenly attacks sperm or embryos, or genetic incompatibilities between partners may interfere with pregnancy.
When to See a Fertility Specialist for Unexplained Infertility
If you’ve been trying to conceive for over 12 months (or 6 months if you’re over 35) without success, it’s important to consult a fertility specialist. They can help identify subtle problems that may not appear in basic tests.
Early intervention often improves outcomes, especially as female fertility declines with age.
Diagnostic Tests for Unexplained Infertility
When standard tests come back normal, doctors may suggest more advanced fertility testing to dig deeper into potential causes.
Hormone Testing:
A detailed hormonal panel helps assess reproductive health:
- AMH (Anti-Müllerian Hormone): Indicates ovarian reserve (number of eggs left).
- FSH & LH: Help understand ovulation function.
- Estradiol: Monitors egg development.
- Thyroid & Prolactin levels: Imbalances here can impact fertility.
Ultrasound & Sonography:
A transvaginal ultrasound examines the uterus and ovaries for fibroids, cysts, or irregularities. Sonohysterography gives a clearer image of the uterine lining and cavity.
Hysterosalpingography (HSG):
A special X-ray to check fallopian tube blockages and uterine abnormalities using contrast dye.
Laparoscopy:
A minimally invasive surgical procedure where a camera is inserted into the abdomen to check for endometriosis, adhesions, or pelvic inflammation, conditions often missed in other tests.
Advanced Sperm Analysis:
Beyond a routine semen analysis, DNA fragmentation tests assess sperm DNA health and can uncover issues not seen in standard reports.
Endometrial Receptivity Analysis (ERA):
This test determines the optimal implantation window, revealing if the uterine lining is ready to accept an embryo.
Emotional Impact of Unexplained Infertility
Unexplained infertility isn’t just a medical diagnosis; it’s an emotional rollercoaster. Couples often feel frustrated, helpless, and anxious because there’s no clear cause or solution.
Common emotional challenges include:
- Feeling out of control due to a lack of answers.
- Relationship stress and emotional distance.
- Social withdrawal due to pregnancy-related conversations.
- Anxiety and depression from repeated failed attempts.
Seeking support from counsellors, support groups, or fertility therapists can help manage this emotional burden and improve mental well-being during treatment.
Treatment for Unexplained Infertility

Even when the cause is unclear, there are effective treatments that can improve your chances of conceiving. Treatment depends on age, duration of infertility, and personal preferences.
Let’s explore the main treatment strategies.
Lifestyle and Natural Optimisation:
Before starting medical interventions, doctors often recommend lifestyle changes that can boost fertility naturally:
- Eat a balanced, antioxidant-rich diet.
- Quit smoking and reduce alcohol or caffeine intake.
- Manage stress through yoga, meditation, or counselling.
- Track ovulation to time intercourse effectively.
Sometimes, these changes alone lead to conception within a few months.
Ovulation Induction (OI):
If natural methods don’t help, doctors may use fertility medications to stimulate ovulation. Common drugs include:
- Clomiphene Citrate (Clomid)
- Letrozole (Femara)
- Gonadotropins (injectable hormones)
These medications increase the number of eggs available for fertilisation, improving the odds of conception.
Intrauterine Insemination (IUI):
In IUI, the sperm is collected, washed, and directly placed inside the uterus during ovulation. This bypasses potential sperm transport issues and increases fertilisation chances.
Success rates for IUI in unexplained infertility are around 10–20% per cycle, depending on age and other factors.
In Vitro Fertilisation (IVF):
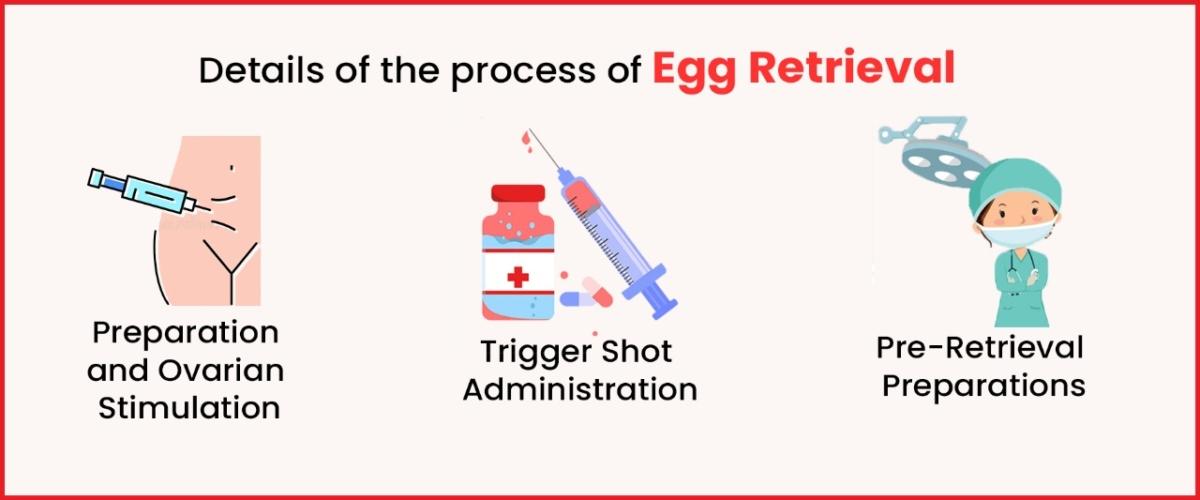
When simpler treatments fail, IVF offers the highest success rates. In this process:
- Eggs are retrieved from the ovaries
- Sperm is collected and fertilised with the eggs in a lab.
- Healthy embryos are then transferred into the uterus.
IVF helps overcome multiple hidden barriers, from sperm-egg interaction issues to embryo development problems.
Intracytoplasmic Sperm Injection (ICSI)
In cases where sperm may not fertilise eggs naturally, ICSI is used. A single sperm is injected directly into an egg, ensuring fertilisation. This is often recommended for couples with unexplained infertility after failed IVF attempts.
Advanced IVF Add-ons
Newer techniques can improve IVF success rates for unexplained infertility:
- Preimplantation Genetic Testing (PGT): Checks embryo chromosomes for abnormalities.
- Time-lapse imaging: Monitors embryo growth for optimal selection.
- Endometrial Scratch: May improve implantation chances in some cases.
- ERA test-guided embryo transfer: Ensures embryo placement during the most receptive window.
Success Rates for Unexplained Infertility Treatments
Success varies depending on age, health, and chosen treatment:
| Treatment Type | Average Success Rate Per Cycle |
| Lifestyle Changes & Timed Intercourse | 5-10% |
| Ovulation Induction + intercourse | 10-15% |
| IUI with Stimulation | 15-20% |
| IVF | 40-60% |
| IVF with ICSI or PGT | Up to 70% in optimal cases |
Remember, success rates increase when treatment is customised based on individual diagnosis and doctor guidance.
Can You Get Pregnant Naturally After Unexplained Infertility?
Yes, it’s absolutely possible. Around 20–25% of couples diagnosed with unexplained infertility eventually conceive naturally, sometimes even after starting or pausing treatment.
Fertility specialists often encourage couples to balance medical treatment with emotional wellness, as stress reduction and lifestyle improvements play a big role in fertility outcomes.
How to Cope with Unexplained Infertility

While the journey may feel uncertain, here are a few ways to stay strong:
- Educate yourself; understanding your condition reduces anxiety.
- Seek support from fertility counsellors or online communities.
- Celebrate little progress (like improved test results or regular ovulation).
- Take breaks between treatments if needed; emotional recovery is crucial.
- Maintain intimacy beyond the fertility schedule to strengthen your relationship.
Conclusion – Unexplained Infertility
Unexplained infertility may feel like a mystery, but with the right guidance and advanced fertility care, your journey to parenthood can still have a happy ending. Today, reproductive medicine has evolved to uncover hidden causes and offer effective solutions through treatments like ovulation induction, IUI, IVF, and ICSI.
At Imprimis IVF, we understand that every couple’s journey is unique. Our expert fertility specialists combine cutting-edge technology, personalised treatment plans, and compassionate care to help you achieve your dream of becoming parents, even when the cause of infertility remains unexplained.
With state-of-the-art facilities across Srinagar, Jammu, and Bhubaneswar, Imprimis IVF offers convenient access to world-class fertility treatments, advanced diagnostic testing, and emotional support, all under one roof.
No matter where you are in your fertility journey, Imprimis IVF stands beside you with hope, science, and care. Because sometimes, the right support can turn “unexplained infertility” into “unexpected joy.”
Imprimis IVF Centre Branches: –
Best IVF Centre in Srinagar, Kashmir