Insider’s Perspective: What to Expect During IVF Procedures at Imprimis IVF
In Vitro Fertilization (IVF) is famous for infertility treatment and gives hope to couples who cannot conceive. During IVF, eggs are carefully collected from a woman’s ovaries and combined with sperm outside her body to overcome many fertility barriers. Imprimis IVF Centre Srinagar is a beacon of excellence in infertility treatment across Srinagar. Imprimis IVF has a sympathetic group of doctors and employees. They guide couples throughout their journey toward becoming parents through infertility treatment. This article aims to give an insider view of how Imprimis IVF Srinagar conducts its IVF procedures.
Understanding IVF Procedures
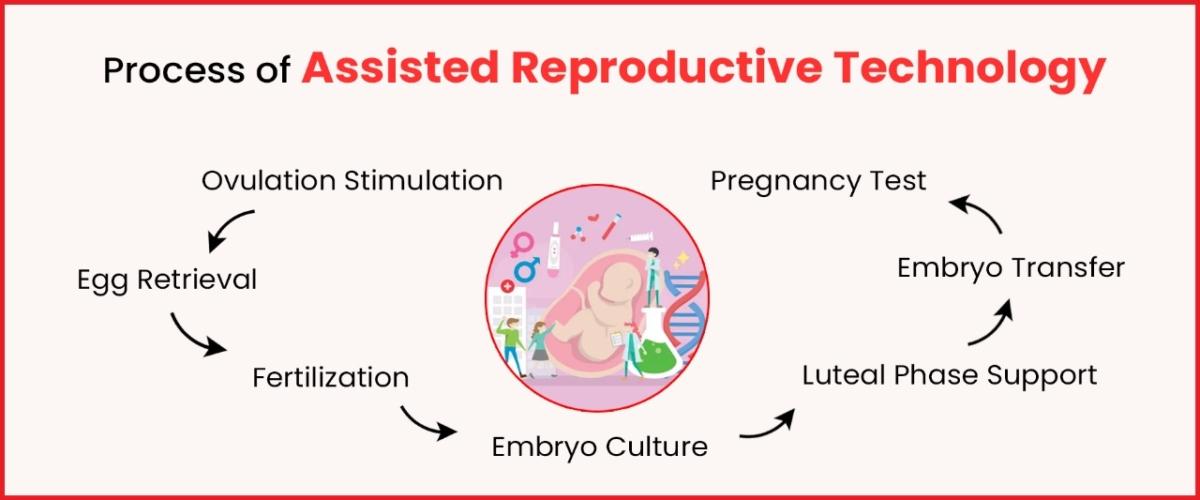
When a couple is considering infertility treatment, they must understand what IVF entails. It starts with a first appointment at Imprimis IVF Srinagar, an IVF centre. Then comes the rest of the journey, which happens in several stages. The first step is Ovarian stimulation, whereby medicines are given to cause ovaries to produce several eggs. Subsequently, these eggs are collected via surgery, albeit minor. After egg retrieval, sperm is added to the eggs, forming an embryo in a laboratory. These embryos are then carefully monitored and cultured to stimulate their growth under controlled conditions. Finally, some selected embryos that seem most promising are transferred into the uterus, hoping they will implant there and can lead to pregnancy if successful.
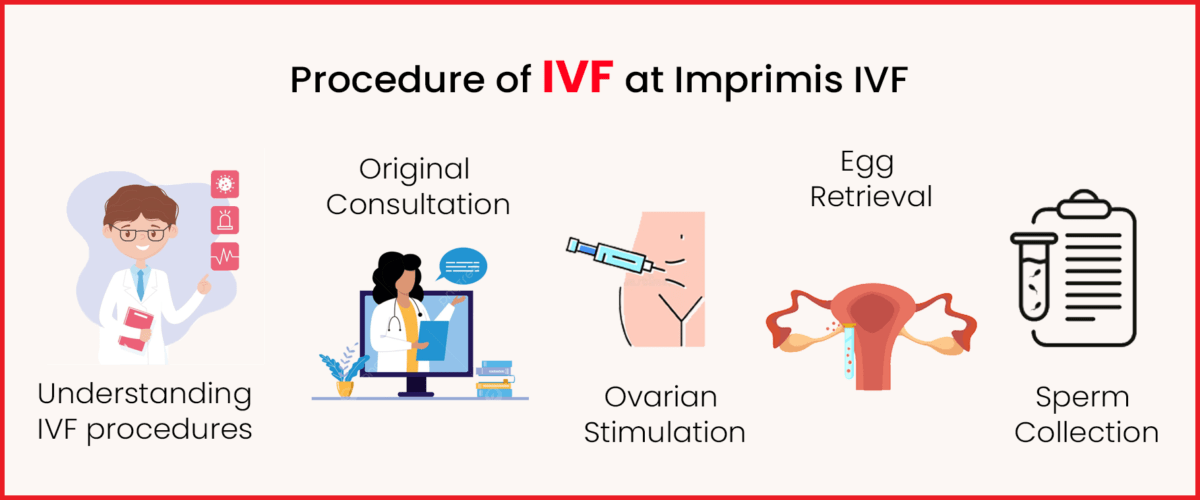
Original Consultation and Appraisal
Imprimis IVF Centre Srinagar begins the in vitro fertilization approach with a comprehensive review. This initial assessment comprises of:
- Medical history
- Fertility status
- Overall health
This evaluation is vital because it helps develop a personalized infertility treatment plan that will maximize chances for success while minimizing associated risks.
Ovarian Stimulation
In the IVF process at Imprimis IVF Centre Srinagar, ovarian stimulation is a significant step. It is a process that involves the use of drugs to induce ovulation of several eggs and hence increase the chances of successful fertilization and implantation. These medications for ovarian stimulation include:
- Gonadotropins
- GnRH agonists.
- GnRH antagonists
At Imprimis IVF Center Srinagar, the medical team will monitor your response to these medications through frequent ultrasounds and blood tests to ensure that your ovaries are responding well and minimize the risk of OHSS.
Egg Retrieval
It is an essential milestone in the process of IVF at Imprimis IVF Centre Srinagar when the transvaginal oocyte retrieval procedure is conducted. It involves taking out fully developed eggs from ovaries to be fertilized. This process, which does not require any cutting through the skin, is usually done with sedation or anaesthesia for the comfort and safety of the patient. The doctor will guide a thin needle using ultrasound scanning into each follicle and then suck out fluid containing the eggs by aspiration, which takes approximately 30 minutes only. After this step of infertility treatment, all recovered eggs are transferred into a laboratory for further processing.
Sperm Collection and Preparation
From all forms of procedures performed at Imprimis IVF Center Srinagar, sperm collection and preparation stand out as crucial during an IVF process. The spouse gives his semen sample, which is later treated to separate the best sperm that can fertilize an egg cell collected from a woman’s ovary after extraction. It can be done through sperm washing, where sperm isolated from the seminal fluid becomes ready to create embryos by being implanted in recovered eggs. It affects how successful the whole IVF infertility treatment may be.
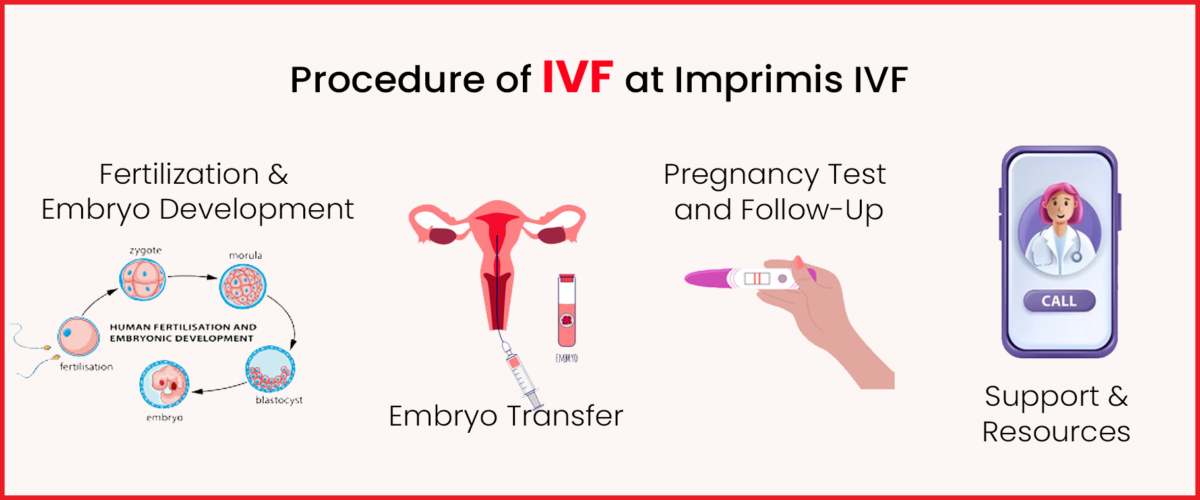
Fertilization and Embryo Development
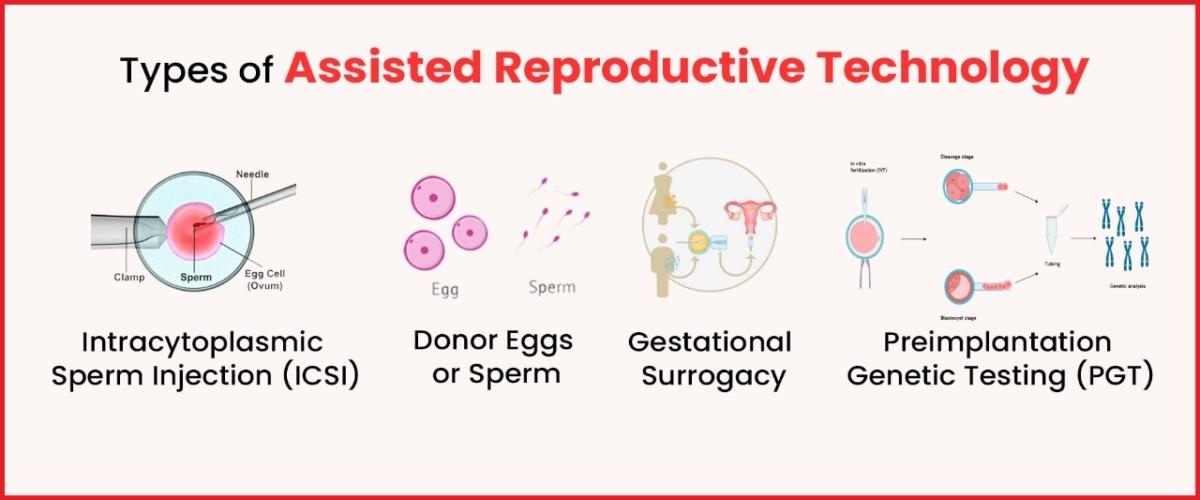
Once the eggs are collected and sperm is prepared, the next phase of the Imprimis IVF Center Srinagar IVF infertility treatment process involves the fertilization of these eggs by processed sperm in labs. It usually happens either through insemination or intracytoplasmic sperm injection method (ICSI), where a single sperm is directly injected into an egg. After this, the produced embryos are observed for a few days to check if they can be implanted successfully in the womb.
Embryo Transfer
The most viable embryos that have been developed well enough are selected for being transferred into the uterus in the process of infertility treatment. Under ultrasound guidance, this gentle procedure is done to place them in a position that would facilitate implantation and establish pregnancy successfully. The number of embryos that will be transferred takes into account several factors, including quality and age of the patient, to increase the chances of successful pregnancy without increasing chances for multiple gestation.
Pregnancy Test and Follow-Up
About a fortnight later, the embryo transfer process will have to be followed by a pregnancy test done to ascertain the efficacy of the procedure. If it is positive, then the patient will go on with check-ups that are supervised during her pregnancy period for the best outcomes ever. Typically, this entails consistent ultrasound testing, blood analysis, and other evaluations meant to ensure the growth and well-being of both mother and infant. Imprimis IVF Center Srinagar provides complete care and support for patients throughout their journey in IVF infertility treatment, including early pregnancy stages.
Support and Resources
Imprimis IVF Centre Srinagar recognizes that the journey to parenthood can be difficult, so we provides a full range of support services to help couples at every step. The Center’s committed team conducts counselling where couples express their concerns, dreads, and wishes in a non-judgmental atmosphere. Moreover, Imprimis arranges group therapy sessions for couples who can interact with others sharing similar experiences, offering mutual comfort and empathy. From emotional support to practical advice to educational materials, there is always something here for each couple in need during this challenging period.
Success Rates in Imprimis IVF Srinagar
Imprimis IVF Centre Srinagar feels proud of its high success rates, showing its commitment to excellence in fertility care. Through its robust IVF procedure, Imprimis attains its success through a combination of modern technology, experienced medical staff with compassion for the patients, and an individualized patient approach. Every couple is unique, so This IVF Center customizes its infertility treatment plans to address specific needs and circumstances. Imprimis’ patients are guaranteed success since it combines advanced techniques with personalized care.
Conclusion
We have covered all the necessary information about this article. Ultimately, the goal of IVF infertility treatment is to help people achieve their dream of starting or expanding their family, and understanding the costs involved is a crucial step in that process. You can also visit our IVF Center’s official website for more information about IVF procedures.