Erectile Dysfunction: Symptoms, Causes, Diagnosis and Treatment
Erectile dysfunction is a condition that occurs when a man cannot achieve or maintain an erection during sexual intercourse to his satisfaction. This problem affects many men all over the world who may have physical, emotional, or lifestyle backgrounds. Many of these conditions can be well managed if dealt with properly.
By addressing physical health issues, offering emotional support, and seeking treatment, people and couples can prevent ED through recovery and regain sexual pleasure as well as general health. The process of recovering from ED involves working together, understanding each other, and collaborating with the therapist until one regains confidence and enjoys life.
What Causes Erectile Dysfunction?
There can be many factors causing erectile dysfunction, some of them may be:

1. Physical Factors:
Vascular Factors:
Some diseases that affect blood flow to the genitals include hardening of arteries (atherosclerosis), high blood pressure and high blood sugar levels (diabetes mellitus) which can result in impotence. These disorders prevent blood vessels from dilating properly and supplying enough blood to the genital area for stimulation during sexual arousal.
Neurological Disorders:
Examples of nervous system conditions that could have an impact on the functionality of erection include multiple sclerosis, Parkinson’s disease, and spinal cord injury which prevents sperm data transmission and blood cells to the brain.
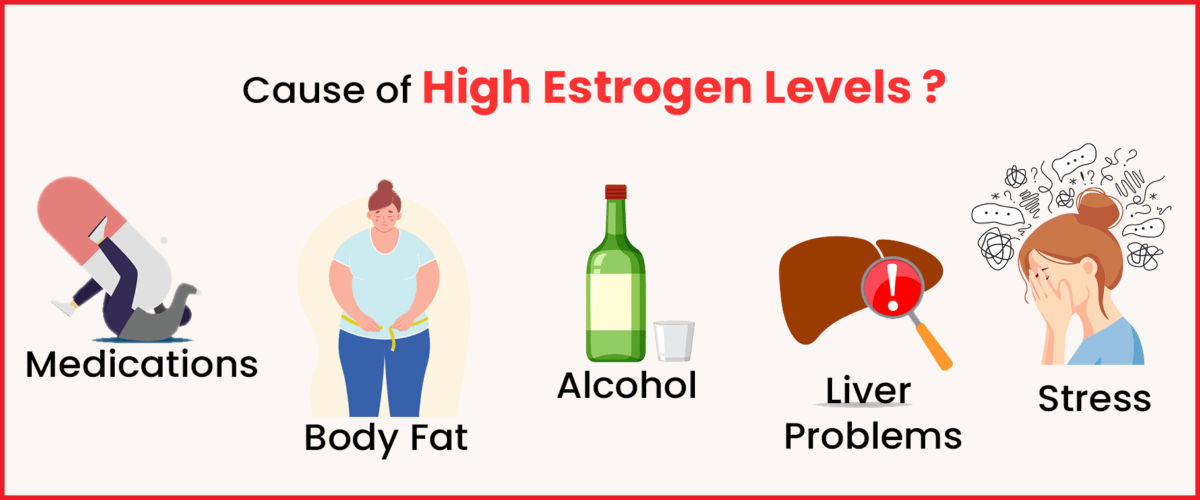
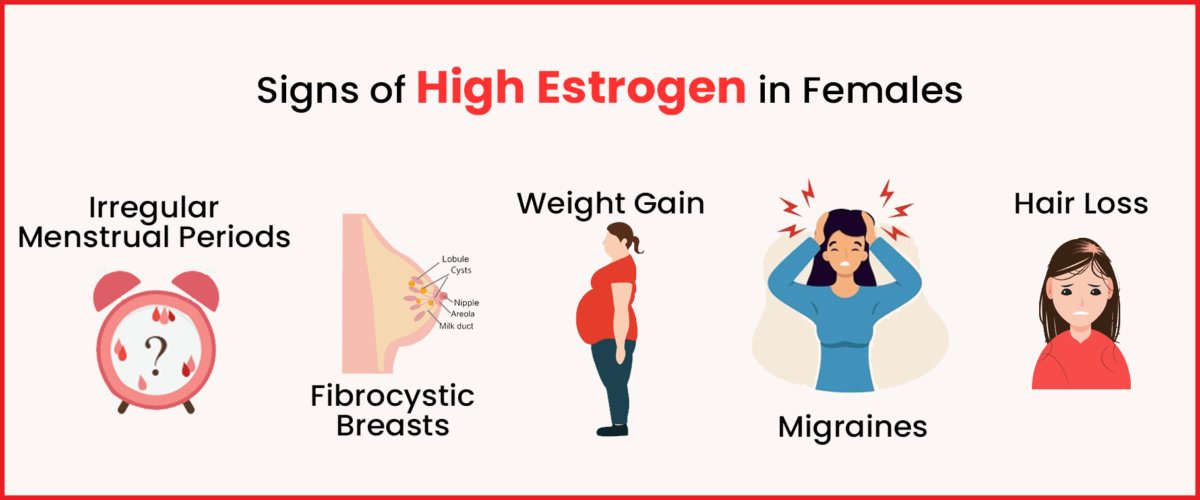
Hormonal Imbalances:
Decreased libido (sexual desire) can be caused by low testosterone levels in males resulting in erectile dysfunction. For example, hypogonadism (insufficient production of testosterone) or medications or therapies for special conditions might cause hormonal imbalances.
Anatomical Issues:
Also playing a role in erectile dysfunction is the abnormality in the genital area like Peyronie’s Disease (scarring within the genitals) and pelvic trauma (injury to the pelvis).
2. Psychological Factors:
Stress and Anxiety:
Erectile dysfunction may be caused by psychological stress such as job stress, work-related stress, love-life tension, sexual pressure anxiety etc; all these emotions influence the human mind’s ability to send signals that speed up blood- flow toward the genitals during sexual arousal.
Depression and Mental Health Conditions:
Erection problems are just a few among other issues such as depression and mental health conditions which would also affect hormone levels and influence male body responses to sex.
3. Lifestyle Factors:
Smoking and Alcohol:
Too much smoking and drinking alcohol can harm blood vessels and other body parts including kidneys. Both long-term smoking and excessive drinking can result in erectile dysfunction by reducing the blood flow as a whole leading to heart disease.
Fatness:
Weight gain or weightiness is connected with different health problems like diabetes, hypertension, and coronary artery disease all lead to erectile dysfunction in men.
Lack of Exercise:
Inactivity that comes alongside a sedentary way of life will result in obesity-related issues like cardiac situations among others which are normally associated with E.D. (erectile dysfunction). On the other hand, physical activity aids in the maintenance of an adequate flow as well as circulation for erection purposes.
Diagnosis and Treatment of Erectile Dysfunction

Diagnosis of erectile dysfunction often implies an extensive medical assessment which involves physical examination, taking down a patient’s records, and in some cases special tests like blood examinations to check hormones or measure the blood flow to the genitals.
1. Medical Evaluation:
Physical Examination:
The doctor will assess the semen and testicles for any physical malformations and evaluate general health.
Medical History:
Inquiring about symptoms, previous treatment, medications, and lifestyle may help one find out what is causing erectile dysfunction.
Laboratory Tests:
These can include blood investigations that are useful in diagnosing such conditions as diabetes, heart disease or hormonal imbalances that may cause erectile dysfunction.
Psychological Evaluation:
It may be necessary to address stress, anxiety, depression and other emotional states that could play into erection problems.
2. Treatment for Erectile Dysfunction:
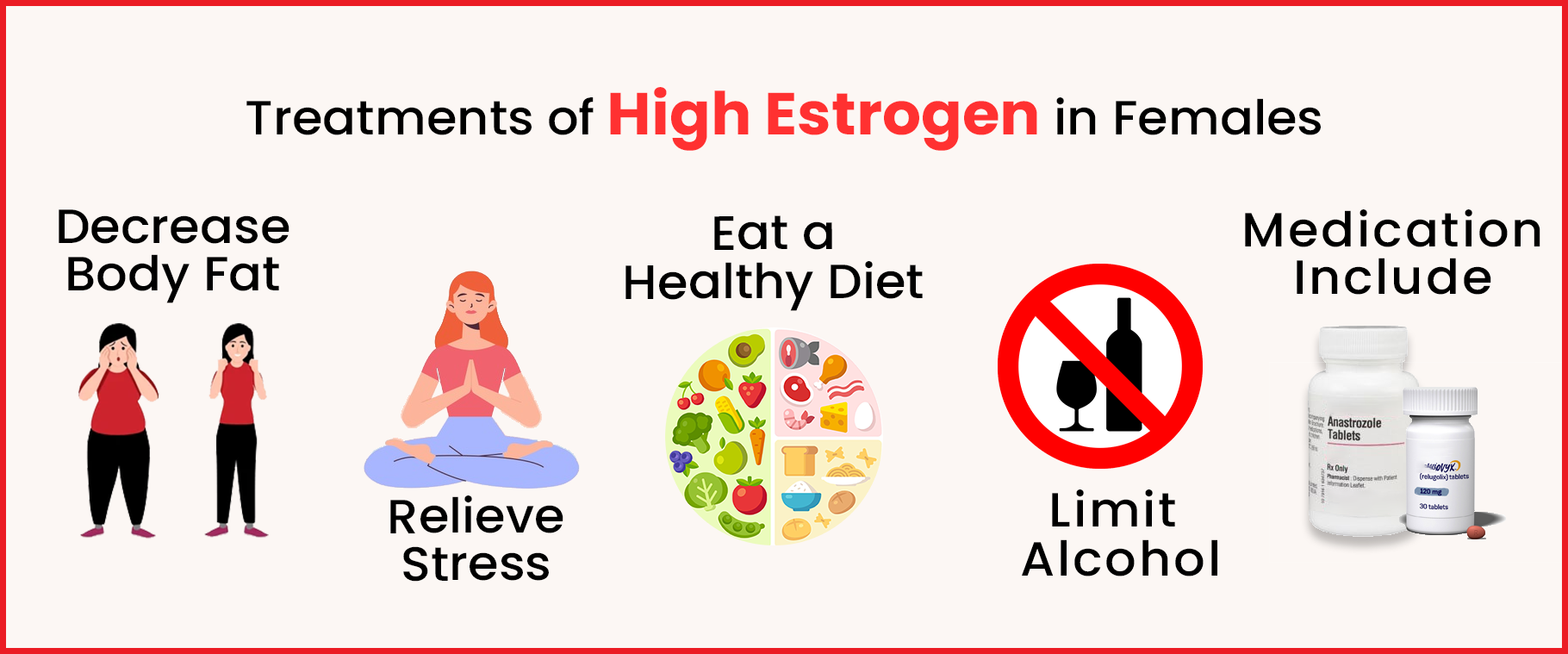
Changes in Lifestyle:
Making healthy lifestyle changes like getting a healthier diet, exercising more, quitting smoking, and drinking less alcohol can improve your overall health as it could naturally reverse erectile dysfunction.
Medicines:
There are several oral medications like
- Sildenafil (Viagra)
- Tadalafil(Cialis)
- Vardenafil (Levitra)
- Avanafil (“Stendra”)
which needs the bloodstream to centre around the penis for better erections. These drugs are used to have better intercourse and they work with an erection half an hour before having sex.
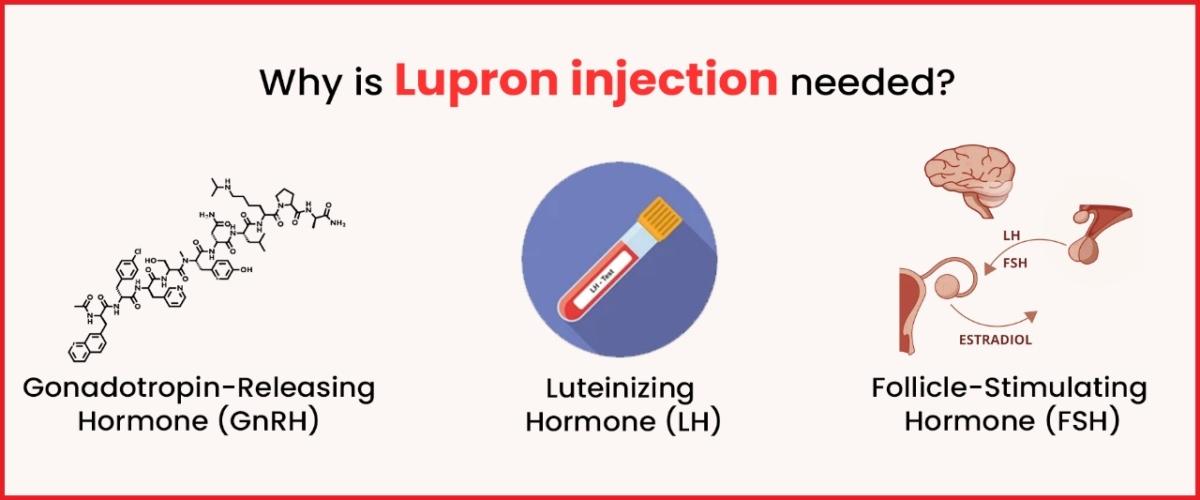
Hormone Therapy–
If low levels of testosterone are responsible for the ED, in such cases doctors will recommend undergoing hormone therapy replacement.
Psychological Counselling:
Therapy or counselling may be beneficial for men suffering from erectile dysfunction as a result of psychological issues (stress, anxiety, depression).
Vacuum Devices and Penile Implants:
For men who do not respond to other treatments, devices such as a vacuum erectile dysfunction device (VED) or surgical options such as penile implants may be considered. This device provides a solution to men who can no longer achieve erection by creating an erection mechanically or surgically.
Psychological Impact of Erectile Dysfunction:
Erectile dysfunction can have a significant impact on a man’s self-confidence, relationships, and overall quality of life. Anxiety, shame, and feelings of powerlessness are common in men with erection problems. Additionally, partners may feel anxious and unsure about their relationships. Open communication, support from doctors, and treatment options based on individual needs are important for addressing the psychological effects of erectile dysfunction and confidence in sex.
Frequently asked questions
Q. What is Erectile Dysfunction (ED)?
A. ED is a condition where a man has difficulty getting or maintaining an erection firm enough for sexual activity. It can be a source of stress and affect relationships.
Q. What causes Erectile Dysfunction?
A. ED can be caused by a variety of factors. Common causes include underlying health conditions like heart disease, diabetes, high blood pressure, or psychological factors such as stress, anxiety, or depression. Lifestyle factors like smoking, alcohol use, and obesity can also contribute to ED.
Q. How is Erectile Dysfunction diagnosed?
A. Diagnosis of ED typically involves a physical exam, a discussion of medical history, and possibly blood tests to check hormone levels, cholesterol, and blood sugar levels. In some cases, specialized tests like ultrasound or overnight erection tests may be recommended.
Q. Can Erectile Dysfunction be treated?
A. Yes, there are several treatment options for ED. These can include oral medications like Viagra or Cialis, lifestyle changes such as exercise and diet modifications, counselling or therapy to address psychological factors, vacuum devices, penile injections, or in more severe cases, surgery.
Q. Is Erectile Dysfunction common?
A. Yes, ED is a common condition, especially among men over 40. It’s estimated that about 50% of men between 40 and 70 years old experience some form of ED at some point.
Conclusion:
Many factors are responsible for erectile dysfunction and these come under body, mind as well lifestyle. This is not a natural part of ageing, but it tends to get worse as we grow older. It is necessary for early recognition and treatment, which can help restore erectile function thus improving sexual health. It will help you go through the causes of your condition, lifestyles that need to be changed and available treatments for managing erectile dysfunction and improving your life.
Imprimis IVF the best IVF Centre in Srinagar, offers hope in the treatment of infertility and ED. We provide innovative reproductive solutions along with individualized treatment. Being among the top IVF clinics in Srinagar, we take great pride in our dedication to quality in all facets of our work. We at Imprimis IVF & Fertility Centre recognize the significance of your desire to begin a family. Together, you and our skilled fertility specialists create a personalized treatment plan that meets your individual needs.