10 Factors That Determine Your IVF Success Rate
In-vitro fertilization (IVF) is a frequently utilized strategy that aims to assist couples in conceiving when natural approaches have not proven effective. Achieving success through IVF is critically important. Determining the IVF success rate and understanding how it is calculated can help provide perspective and realistic expectations to prospective patients.
The success rate considers the percentage of IVF treatment cycles that lead to a confirmed pregnancy, which results in a live birth. It is impacted by multiple factors, including the age of the female partner, the cause of infertility, the number and quality of embryos transferred, and whether embryos have been previously frozen through the IVF process.
The IVF success rate is determined by dividing successful pregnancies by the number of IVF cycles performed. It’s often shown as a percentage. However, other factors affect IVF success, and patients need too and to know about them before starting IVF. Here we look at the top 10 factors that determine your IVF success.
Common Factors that Call for Successful IVF
Among other important lists of factors for successful IVF, we have pointed out the top 10 that are probably the most important ones. Here are some of the factors that influence IVF success rate:
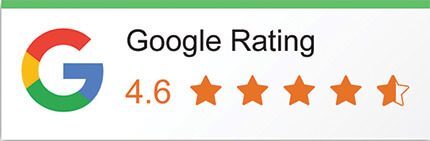
1. Age of the Patient
A person’s age is an important factor in determining the appropriate in vitro fertilization, or IVF, process, especially concerning the utilization of donor eggs. For many individuals, their eggs are employed, however, if one is over the age of forty, incorporating donor eggs has the potential to elevate the likelihood of success. While still relying on one’s biological material is usually preferable, the decline in egg quality that naturally accompanies advancing maternal age means those in their forties may want to take donor eggs into account as a viable option worth exploring.
Between the ages of 24 and 34, women have among the best chances of achieving success with in vitro fertilization, or IVF, as this period is typically viewed as the peak years of fertility. However, once a woman reaches 40 years old, the likelihood of a successful pregnancy through IVF treatment decreases. The 24 to 34 age group is considered the time of highest natural fertility when the quality and quantity of a woman’s eggs are at their prime.
As a woman ages past 35, both egg quantity and quality decline steadily each year. This is due to the natural ageing process of the ovaries over time. While IVF provides an opportunity for pregnancy beyond a woman’s natural fertile window, the odds of bringing home a baby continue to diminish the older a woman is when she begins treatment.
2. Previous Pregnancy
Having experienced a successful pregnancy previously provides hope that in vitro fertilization (IVF) may be successful again, as the woman’s body has demonstrated its ability to support a healthy pregnancy and deliver a baby full-term. However, if prior IVF attempts or miscarriages are numerous, the likelihood of achieving a successful pregnancy may decline.
After all, each failed cycle or loss reduces the chances with each subsequent try. Still, medical advances continue and each new cycle brings a fresh opportunity, so it is important patients work closely with their doctors to optimize chances through customized treatment plans.
3. Fertility Issues
The nature of the fertility challenge holds significance. Certain difficulties can be more arduous to address than others, impacting both individuals and their partners. For example, those with blocked fallopian passages may encounter lower achievement quotas contrasted with people encountering issues with egg discharge. This component extraordinarily affects the achievement rate of the initial IVF treatment attempt. The sorts of fertility issues experienced can decide the seriousness of treatment and the prospects of achievement on the principal endeavour.
Blocked tubes regularly make it harder for eggs to meet sperm, bringing down the probability of standard conception. On the other hand, issues with ovulation regularly just require a prescription or different methods to trigger egg discharge, accomplishing pregnancy effectively. While each case merits individual consideration, understanding how the sort of issue influences the test of treatment can assist couples with choosing the most suitable course and setting sensible desires.
4. Quality of the Eggs and Embryos
Several aspects can impact the quality of eggs and embryos during in vitro fertilization, or IVF, treatment including a woman’s age, ovarian reserve, the stimulation protocol used, and sperm quality. Eggs and embryos of higher quality present a greater potential for success with IVF.
One of the most crucial factors is a woman’s ovarian reserve, which refers to the number of eggs in her ovaries. This has a direct impact on egg quality. Younger women are likely to produce maternal cells of better quality than those who are not in good ovarian reserve. Fertility medications that help eggs grow and ripen can alter quality. The stimulation procedure is the culprit. Several procedures might result in that.
5. Quality of the Sperm
The vast majority of chromosomal issues found in embryos, approximately 90%, are attributable to egg quality. However, male fertility problems also influence embryonic development. Scientific progress has provided valuable tools to mitigate these influences, raising the likelihood of achieving a healthy pregnancy.
While female reproductive health accounts for most chromosomal abnormalities observed in embryos, male factor infertility poses challenges as well. New technologies are helping to reduce the impact of these influences and boost the chances for successful conception. Further advancements in assisted reproduction hold promise for additionally lessening the effects of egg and sperm deficiencies, potentially aiding many hoping to start a family.
6. COH (Controlled Ovarian Stimulation) Protocol
After considering the woman’s age and hormonal levels, along with other health conditions, the doctor will decide on a suitable tolerance treatment plan. Usually, this plan involves medications, ranging from 10 to 14 days, during which growth is stimulated with the aid of hormonal monitoring, frequent blood tests, and ultrasound.
If the yield is disappointing with most eggs not reaching maturation, the current cycle which is in the production process may, therefore, be discontinued. In this example, the medical professionals would then assess what modifications could improve the treatment of the next round by correcting the medicine dose for example.
7. Lifestyle of the Patient:
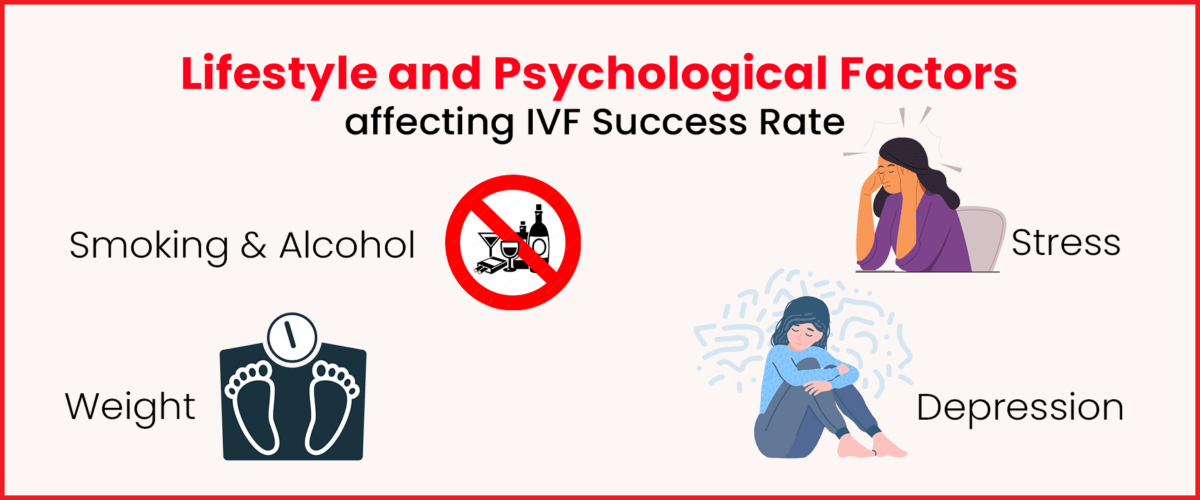
Leading a healthy lifestyle sets the stage for a thriving embryo environment. Before starting IVF, it’s crucial to quit smoking and drinking alcohol for at least three months. Both habits reduce success chances, with smokers having 50% lower implantation rates.
Maintaining a healthy weight also boosts IVF success. Obesity affects hormone processing, fertility medications, menstrual cycles, and carrying a baby to term. The upside is, that you have control over your lifestyle, and these factors can be actively improved.
8. Embryo Transfer
The embryo transfer procedure plays an extremely important role in IVF treatment, according to many specialists in the field. Not only does it require a healthy embryo and successful implantation into the uterus, but the transfer itself must be executed perfectly. The timing and biological conditions involved in this process are critical, as any issues can negatively impact the chances of a successful outcome.
A flawless transfer represents one piece of the larger puzzle, and if done incorrectly, it could undermine the efforts of developing quality embryos and preparing the uterine lining. While physicians work to optimize the many factors within their control, couples also hope mother nature cooperates to allow the embryo’s implantation. Success at this phase means the chance for pregnancy continues, whereas problems may cut the process short. Perfection matters.
9. Uterine Receptivity
A woman’s uterine lining is important in achieving success with in vitro fertilization. For an embryo to successfully implant, the uterine lining must be adequately thickened to support the development of a pregnancy.
Several factors can influence uterine receptivity, making it crucial to optimize the environment within the womb. Hormonal supplements are often prescribed to help strengthen and build up the endometrial lining. Tests such as a hysteroscopy procedure may also be used to examine the uterus and address any issues that could impact implantation.
10. Mental Health
Finally, the last but not the least key to maintaining a positive outlook when experiencing in vitro fertilization is to rate your mental health as anxiety, depression, and stress have been reported by many to seriously affect IVF success rates.
The emotional health of women taking IVF is very critical because cortisol and other stress hormones in large volumes worsen the uterus’s receptivity to implantation and embryo development in the early stages. There are various ways for patients have contribute to the reduction of stress or improvement of their mood condition, such as counselling or therapy. One of the major challenges of mental terms is finding the right words to speak about it.
Conclusion
The IVF Success Rate is determined by various elements, ranging from patients to medical practitioners, and must be addressed collectively. Infertility treatment requires a lot of effort, from our age and the eggs and embryo quality to the way we live and the intricacy of the embryo transfer process; each of these features directly affects our chances for success.
Lastly, dealing with fertility problems, making the uterus more ready for pregnancy, and paying attention to emotional health are some of the measures that play a pivotal role in making the IVF treatment journey much more successful. The successful implementation of these troubleshooting factors will help patients approach IVF treatment with a more realistic approach and increase confidence, as they will know that they are taking the necessary steps to achieve their dream of being parents.