Asherman Syndrome: Causes, Symptoms, and Treatment
Asherman Syndrome – An acquired illness known as Asherman’s syndrome causes adhesions, or scar tissue, to develop inside your uterus. There may be less room for expansion inside your uterus as a result of the accumulation of scar tissue. This illness may develop as a side effect of cancer therapy or medical procedures. Asherman’s syndrome can cause infertility, pelvic pain, or light or nonexistent periods in women.
What is Asherman’s Syndrome?
Scar tissue, sometimes known as adhesions or intrauterine adhesions, accumulates inside your uterus in a rare illness known as Asherman’s syndrome. Less space is created inside your uterus by this additional tissue.
Imagine a room where the walls grew thicker and thicker, thus reducing the amount of space in the middle. This illness may result in irregular uterine bleeding, pelvic pain, and problems conceiving. Treatment for Asherman’s syndrome frequently results in symptom relief.
IUDs and Asherman’s Syndrome: is it possible?
A kind of long-term birth control called an intrauterine device (IUD) is inserted into your uterus and left there for a certain amount of time, usually several years. There is always a chance of infection and scar tissue formation when this device is inserted into your body. IUDs and Asherman’s syndrome are not frequently associated with one another, while this is not the condition’s known aetiology.
How to identify Asherman Syndrome?
Asherman’s syndrome is usually diagnosed based on symptoms such as pelvic pain, irregular uterine flow, amenorrhea (absence of menstruation), or difficulty becoming and maintaining pregnancy. Asherman’s syndrome may potentially be diagnosed based on your medical history. You might be evaluated for Asherman’s syndrome if you have undergone radiation treatment, a c-section, a dilatation and curettage (D&C) procedure, or a pelvic infection. Asherman’s syndrome can be brought on by any of these treatments or ailments.
Your IVF experts will review your medical history when you book an appointment. Make sure to let your provider know if you have ever had any pelvic surgery that isn’t listed in your medical history. That data may be crucial for the diagnosis of Asherman’s syndrome. After that, your doctor will examine you physically, but first, they will do a sonohysterogram to look for scar tissue inside your uterus. Using a tiny catheter, your doctor will inject a small amount of saline solution into your uterus during a sonohysterogram. After that, transvaginal ultrasonography is used to check for tissue blockages in the cervix or cavity.
Which tests are appropriate for the diagnosis of Asherman Syndrome?
Your IVF specialist can view your interior organs thanks to imaging tests. Different tests offer varying levels of specificity. These tests can be simple procedures performed on top of your skin with little to no preparation, or they can be more involved.
The following imaging tests can be used to identify Asherman’s syndrome:
1. Ultrasound
This kind of imaging exam makes an image of your interior organs by using sound waves. You can have an internal transvaginal ultrasound or an external ultrasound performed on your skin. This variation of the test involves inserting a thin wand into the vagina.
2. Hysteroscopy
This procedure involves your doctor seeing inside your uterus with a thin tool that has a camera on the end. This is placed in your vagina and advanced into your uterus via your cervix. With a hysteroscopy, your doctor may look into your uterus in great detail. It can be applied to the management of Asherman’s syndrome.
3. Saline Infusion Sonography
To get a clear image of the inside of your uterus, this imaging procedure combines ultrasound technology with a saline solution, which is a solution of salt and water. Your uterus expands as a result of the fluid, allowing your healthcare professional to observe the specifics of the structure and flaws in your uterus.
What Is The Impact of Asherman Syndrome on Fertility?
It could be difficult for you to become pregnant if you have Asherman syndrome. The likelihood of miscarriage is considerable if you do. Although there is no room for fetal growth due to adhesions in the uterine walls, it is possible to become pregnant despite suffering from the condition.
This increases the likelihood of miscarriage or stillbirth compared to women without the disease. Pregnancy with Asherman syndrome also increases the chance of certain disorders, such as:
1. Placenta Accreta
The placenta adheres to the uterine wall too firmly. Pregnancy at high-risk results from this. The placenta stays connected after birth in whole or in part, which results in excessive bleeding.
2. Previa Placenta
The cervix’s opening is blocked by the placenta, which can result in heavy bleeding during pregnancy and childbirth. Premature birth is another risk that is increased by it.
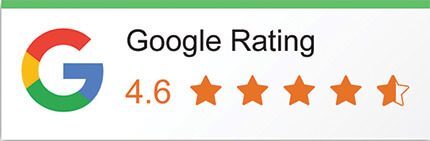
Symptoms of Asherman Syndrome
A rare disorder called Asherman Syndrome affects women’s reproductive systems and results in the development of scar tissue inside the uterus. Many symptoms, such as the following, may result from this scar tissue:
- Amenorrhea, or irregular menstruation
- Consistently losing babies
- Infertility
- Light or absent menstruation
- Pain in the pelvis
- Trouble getting pregnant or repeated losses
Women with Asherman Syndrome sometimes don’t show any symptoms at all, and their menstruation stays regular. On the other hand, the illness may cause problems that arise during pregnancy, including low birth weight, retained placenta, and placenta accreta. Asherman syndrome is typically diagnosed with imaging techniques such as saline sonography, hysteroscopy, or hysterosalpingography.
These techniques can assist in determining whether and how much scar tissue is present inside the uterus. In more severe cases, a hysteroscopy or MRI may be required to assess the disease’s extent. Asherman Syndrome can be treated surgically by dilation and curettage (D&C), hysteroscopy, or in certain situations, a total hysterectomy, to remove the scar tissue. To ascertain the best course of action for their unique circumstances, people must speak with their healthcare providers.
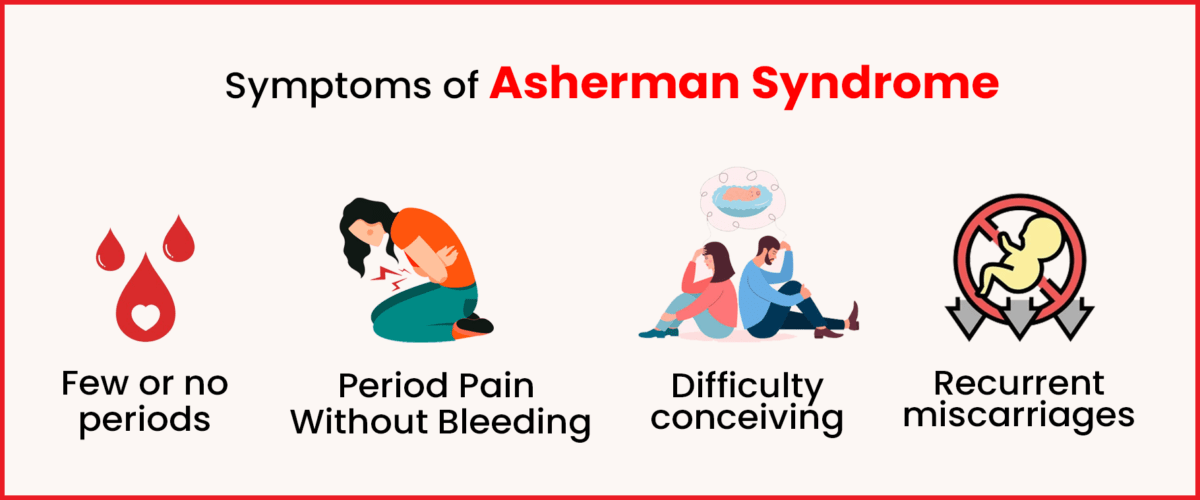
Asherman Syndrome Causes
Asherman Syndrome is a rare condition where scar tissue grows inside the uterus and/or cervix. It’s also called intrauterine adhesions or synechiae. The primary causes of Asherman Syndrome include:
1. Dilation and Curettage (D&C) Procedures
It most often happens after a D&C procedure done for voluntarily ending a pregnancy, late or not fully completed miscarriage, or to treat a placenta left over after having the baby.
2. Severe Pelvic Infection
A bad pelvic infection not connected to an operation could also cause Asherman Syndrome.
3. Other Factors
Stickiness in the uterus can also happen after getting sick with tuberculosis or schistosomiasis.
This condition can cause problems like having light or no periods, pain in the lower body area and trouble getting pregnant. It may also lead to repeat losses of pregnancies and issues during childbirth. It can also mess with making babies, increasing the chances of a miscarriage or a baby not being born alive.
Asherman Syndrome Treatment
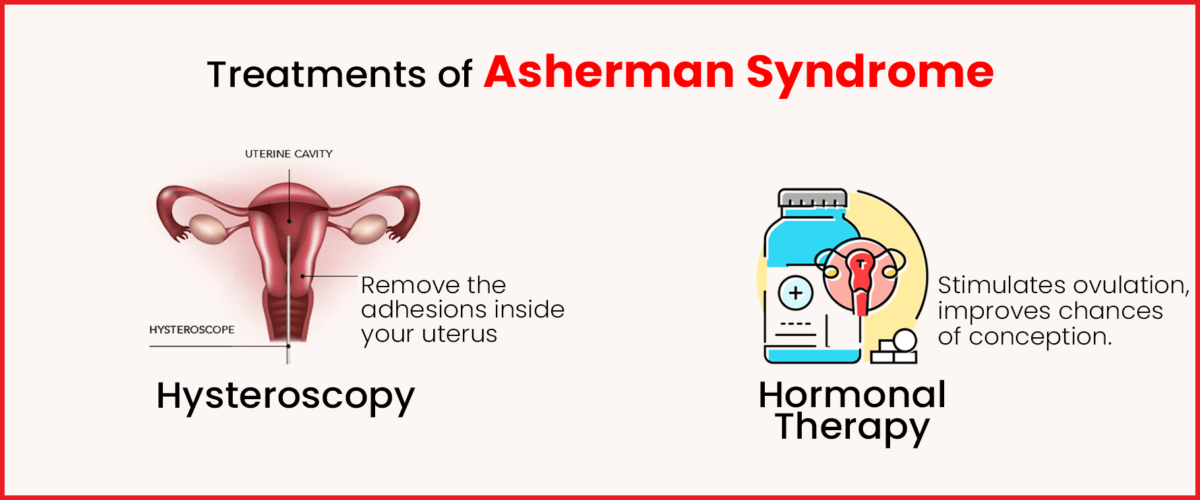
Asherman’s syndrome can be treated in several ways. It’s a good idea to talk about your goals for future fertility as well as how this illness makes you feel, including any discomfort you may encounter, with your healthcare professional. Sometimes the best course of action for a woman who is symptom-free is to do nothing.
On the other hand, there are therapy alternatives that can eliminate the scar tissue if your plan calls for more pregnancies. In addition, treatment may be beneficial if you have pelvic pain or cramps. Removing the scar tissue and getting your uterus back to its normal size and shape is the major objective of treatment. Help for Asherman’s syndrome treatment can include:
- Ease discomfort.
- Return your menstrual cycle (periods) to normal.
- If you are not yet menopausal, permit yourself to become pregnant.
Hysteroscopy
may be used by your doctor to remove the adhesions inside your uterus. During a hysteroscopy, your doctor looks inside your uterus using a thin instrument called a hysteroscope. Scar tissue can also be eliminated with this instrument. The hysteroscope is passed via your cervix, into your uterus, and your vagina. During this process, scar tissue is removed with extreme caution. While the scar tissue is being removed, there is a chance that the surgery will damage good tissue inside your uterus.
Hormonal Therapy
For a few days following the hysteroscopy, a tiny intrauterine catheter may be left inside your uterus in addition to hormonal therapy (estrogen). This will lessen the possibility that scar tissue will regrow following the surgery. Estrogen encourages the healing of your endometrium, which is the inner lining of your cavity, and the catheter creates a physical barrier between your anterior and posterior uterine walls to prevent adhesions in the days that follow the scar tissue removal surgery. Antibiotics will be administered to you to avoid infection during the insertion of an intrauterine catheter.
In Summary
Scar tissue forms inside the uterus in Asherman Syndrome, a rare and acquired disorder that can cause light or nonexistent periods, pelvic pain, infertility, recurrent miscarriages, and irregular menstruation, among other symptoms. The illness is frequently contracted as a consequence of cancer therapies, infections, or surgical operations. It might be difficult to identify Asherman Syndrome because some people may not show any symptoms at all.
Surgery to remove adhesions or scar tissue is the main treatment for Asherman Syndrome; this is usually done using hysteroscopy. Estrogen therapy is frequently used in conjunction with this operation to aid in the uterine lining’s healing and regeneration. Preventive and restorative procedures, like implanting devices to stop scar formation, may be taken into consideration in more severe situations. Many hospitals like Imprimis IVF are suitable for these treatments. It is one of the best hospitals for this. If you need any help, Imprimis IVF can help you.